Navigation links
Free Consultation
It's important to know that you are not alone. Get help with depression today!
TMS THERAPY SUPPORTS MENTAL WELLNESS
- Depression
- Lack of Joy
- Sadness and Despair
- Low Mood
- Lethargy
- Insomnia
- Oversleeping
- Social Isolation
- Self-Harm
- Substance Abuse
- Suicidal Ideation
- Alcoholism

How Do Ketamine and Spravato (esketamine) Work?

Ketamine and esketamine work for depression through a different mechanism
than other antidepressant drugs. Conventional antidepressants increase levels of
naturally occurring chemicals such as serotonin, norepinephrine, and dopamine.
These chemicals are messengers that relay communication between brain cells.
The theory is that greater quantities of these neurotransmitters allow better
communication between brain cells, positively affecting mood. Ketamine and
Esketamine block NMDA receptors in the brain, thereby increasing levels of
glutamate, the most abundant chemical messenger in the brain. Blocking NMDA
receptors also activates AMPA receptors to release other molecules that help
brain cells communicate with each other along new pathways. Known as
synaptogenesis, this process likely affects mood, thought patterns, and cognition.
What Is the Difference Between Ketamine and Spravato (esketamine)?
What Is Ketamine?
You may be familiar with ketamine as an anesthetic that was commonly used on
battlefields or as a veterinary drug. A much lower dose of ketamine is given for
depression compared with the dose necessary for anesthesia. This type of
Ketamine is racemic ketamine, a mixture of “R” and “S” ketamine. It was previously
approved by the Food and Drug Administration to be used as an anesthetic but
has not been approved as a treatment for depression. In addition, the American
Psychiatric Association found that there is not enough information about the use
of ketamine to treat MDD and TRD. There is not sufficient information because
ketamine is old, and pharmaceutical companies have chosen not to dedicate
millions of dollars to clinical trials for ketamine to be used as a depression
treatment.
Ketamine is usually administered intravenously because it metabolizes too fast
when given orally, and the effects are reduced. While the intravenous method is
often effective and provides rapid results, patients have to receive treatment as
much as three times a week and repeatedly have IV lines inserted, which is costly
and can be inconvenient to patients.
What Is Spravato (esketamine)?
Spravato is the brand name for Esketamine. It is a different version of ketamine
that can be administered intranasally and also produces rapid, effective results.
Esketamine is the S form of Ketamine. It is a new development, making
pharmaceutical companies more likely to endorse clinical trials supporting the
use of it. In 2019, the FDA approved the use of esketamine (Spravato) in adults for
the treatment of TRD and MDSI when used in conjunction with an oral
antidepressant.
The safety and efficacy of esketamine (Spravato) are supported by at least three
short-term and two long-term studies. A 2020 study by Papakostas studied the use
of esketamine in 774 people involved in 5 trials. It showed that patients with MDD
or MDSI who received the intranasal esketamine treatments had a better
outcome than those who received a placebo.
Conventional antidepressants may increase suicidal thoughts at the beginning of
treatment, especially in children and young adults. Esketamine (Spravato) is the
only drug besides lithium, a drug commonly prescribed for bipolar disorder, that
is proven to decrease suicidal thoughts.
There are currently no ongoing trials comparing the use of ketamine and
esketamine against each other.
How the Difference Between Ketamine and Spravato (esketamine) Administration Affects You
Esketamine (Spravato) is more potent than ketamine, which allows doctors to give
lower doses and potentially see fewer side effects. Both ketamine and esketamine
must be administered by an RN, PNP, or doctor. These drugs are DEA Schedule III
controlled substances and can become highly addictive.
Ketamine must be administered intravenously up to 3 times a week. This can be
inconvenient and painful as patients have to continue to return to the clinic and
receive a new IV injection each time.
Spravato (esketamine) is administered in an outpatient setting under our RN, PNP,
or doctor supervision. You receive three doses of the medication spaced about 5
minutes apart, and then you remain under supervision for 2 to 3 hours until any
potential side effects have passed.
The side effects for both Spravato (esketamine) and Ketamine can include
- Nausea
- Drowsiness
- Increased blood pressure
- Dissociation (sometimes called out-of-body experiences)
- Headache
The side effects tend to peak at 40 minutes and wear off within two hours of
treatment. You can expect the most intense side effects during the first two
treatment sessions.
Will Insurance Cover Ketamine or Spravato (esketamine) Treatments?
Insurance companies do not cover ketamine treatments because it’s experimental
and not FDA-approved. Therefore, you have to pay out of pocket for it.
Spravato (esketamine) is almost always covered by insurance, including Medicare,
because it is FDA-approved and well-studied to be effective and safe. To be
considered eligible for insurance coverage for Spravato (esketamine), a person
has to have tried at least two other antidepressants without benefit.
Explore Your Treatment Options With Unchained
Wellness Clinic
Ketamine and Spravato (esketamine) are both viable treatments for depression.
When effective, people usually respond within one to three sessions. If a person
has no response after three sessions, further sessions are unlikely to help.
Instead, it’s probably best to try other treatments for depression.
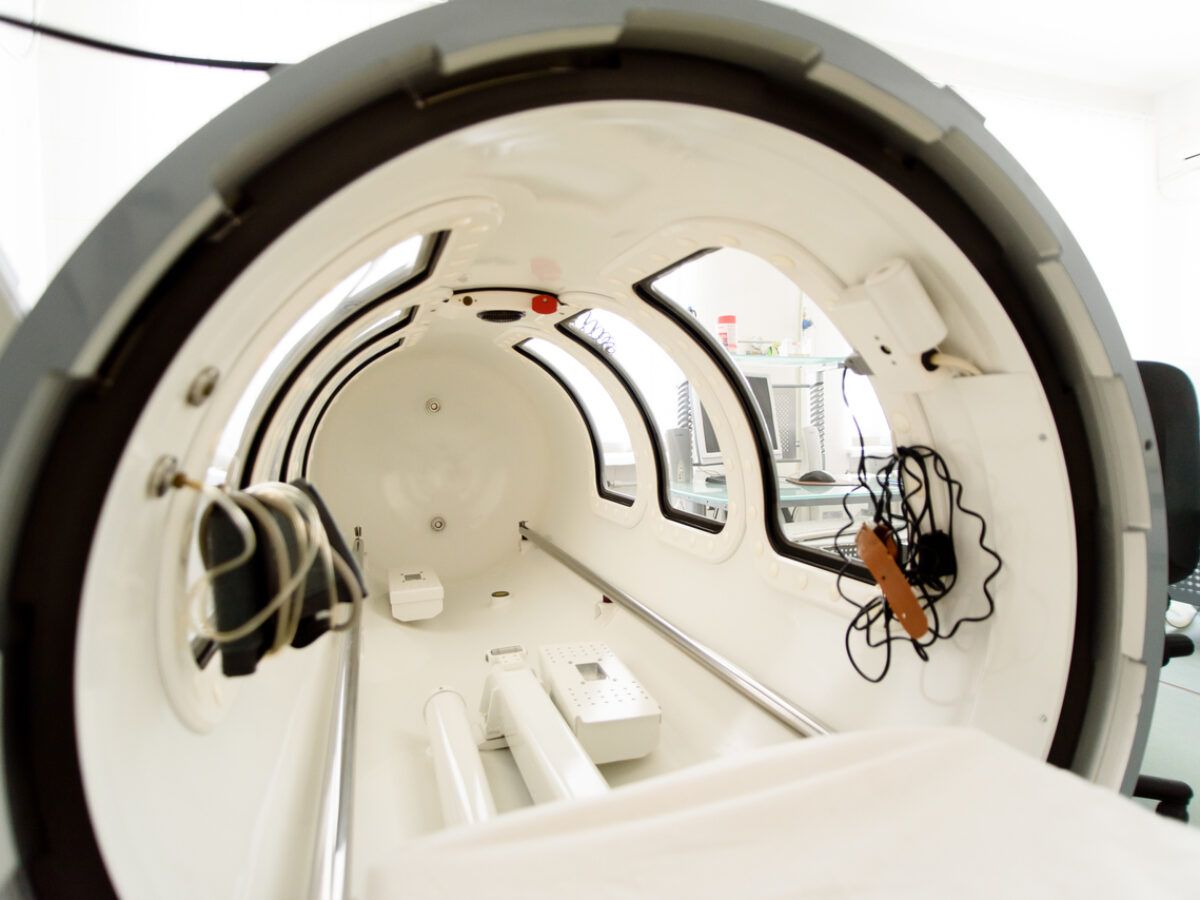
One additional treatment option is TMS (transcranial magnetic stimulation).
TMS is an FDA-approved, noninvasive, highly effective treatment option for people
with MDD. Numerous studies have been performed on the effectiveness and
safety of TMS, and the outcomes have been favorable. At Unchained Wellness
Clinic, we have highly trained professionals who work with the latest technology
and well-researched treatment options to help you feel better by individualizing
the best treatment strategies.
Talk with us today!
Experience transformative relief and reclaim your mental health with our
Ketamine and Spravato treatments at Unchained Wellness Clinic – book your
consult today and discover the path to renewed well-being!